
Blog
Reframing Healthcare Transformation.
Chapter 1: Positive provocations
Over the past 15 years I have had the privilege to collaborate with countless patients, clinicians, CEOs, researchers, designers, and a variety of NGOs. Each system, region and country is different, but the predominant goal is always supporting health systems to be more resilient and financially sustainable.
Our collective achievements in workflow optimization, throughput efficiencies, patient centric design, first time right diagnosis, access to care, and new financing models have all helped to improve overall outcomes. If we look at the progress across our entire industry, there have been startling advances in clinical pathways, image guided therapies, personalized medicine, robotics, and AI which are also radically changing the way healthcare is delivered.
Yet, despite all these amazing and heroic achievements, each day we are all reminded that our global health systems are severely under pressure. Staff shortages and inflation are adding fuel to an increasing demand with limited resources.
As designers, we sit in the crosshairs between technology, business requirements, patient needs and clinical staff requirements. Designers have a duty to question what could and should be the most preferable outcome. This means that we need to start with a holistic view of the challenge and reframe what our objective should be. In the famous words of Knut Yran “Don’t ask a designer to design a bridge over a river, but for a way to cross the river.”
In order to meet the overwhelming challenge we are facing as an industry, we need to move from incremental innovation to designing preferable futures. This series of articles will attempt to do just that. I do not claim to have the answers. My hope is that I can trigger our collective unconscious to help us redefine how we can co-create a more equitable and sustainable health system for us all.
I welcome all comments, contrary views, and personal reflections.
Chapter 2: “The whole is greater than the sum of its parts.” Aristotle
The human biome consists of over one hundred trillion cells. Our bodies are made up of about thirty-five thousand genes with millions of proteins and thousands of metabolites. There are 11 unique biological systems and 78 different organs. This complexity is compounded by the fact that about 70 percent of our cells are made up from the microbiome. We do not sufficiently know how our biological systems work with or impact each other. Genes do not act in isolation, nor is one biological system independent of another. Different proteins may produce different outcomes between diseases or interact quite differently in different systems or across various networks.
Gaining a deep understanding of how biological systems impact each other in the onset and treatment of a disease is critical. There are some areas where there is a growing understanding of the interrelation between diseases. Sleep apnea may cause the onset of a stroke, diabetes, heart disease or potentially cancer. Comorbidity is extremely complex and difficult to decipher because it is in proportion to how many diseases a patient displays and may also include asymptomatic or preexisting conditions.
Patients with comorbidities of more than one disease or condition at the same time are now more prevalent than ever. In 2018, it was estimated that 27% of all US adult patients displayed multiple chronic conditions. From diagnostics to treatment, comorbidities can dramatically exacerbate the impact of a condition. Comorbidity is associated with higher relapse rates, adverse events, and higher mortality rates.
Managing patients with comorbidities needs to take a stronger role in treatment and recovery plans if we are to move towards value-based health care models. Network biology can develop approaches that use genomic and other protein network information to help us better understand the interrelation between diseases. The advancement of AI and quantum computing should enable computational scientists to crack these complex biological codes.
There are many promising areas, but they all require access to our collective personal patient data. The question now becomes not why we should share our data, but rather how can we share our data to help healthcare help us.
Designing a paradigm shift in healthcare.

Our global healthcare system is not sustainable. We are at a real tipping point. Resources are becoming ever limited, while population numbers are rising. We’re lucky enough to be living longer, yet unlucky enough to be suffering a plethora of chronic diseases, often more than one at the same time.
The healthcare system has become so burdened by its enormity that it has neglected an essential need of the customers it so valiantly serves. They want to matter to the experts in whom they place their trust. It’s deeper than wanting to be cared for or cured. It’s a complex emotional bond that’s been fractured.
So how do we fix it? Well, most suggest two solutions. First, government and business can lavish enormous sums of money and attention to patch things up and hope the current system will be elastic enough to support the growing needs. Alternatively, people can make a fundamental change to the way they manage their health, preventing disease and sparking a systemic transformation that benefits citizens as much as the healthcare system.
I believe there is a third, and more preferable way. To co-design a future in which both parties take the initiative and transform each other. Where people are enabled and encouraged to take charge of their own health, to protect and nurture themselves in technologically-advanced ways. Where emboldened healthcare stakeholders take tough, far-reaching decisions that will recalibrate the systems currently crumbling in front of their eyes.
Empowerment is the key behind this extraordinary paradigm shift. And design thinking can be leveraged to unleash those forces for change to fulfil the needs of both system and customer.
Empowered customers can help to redesign a more personalized system, so that instead of feeling like a nameless commodity their own actions and choices will matter.
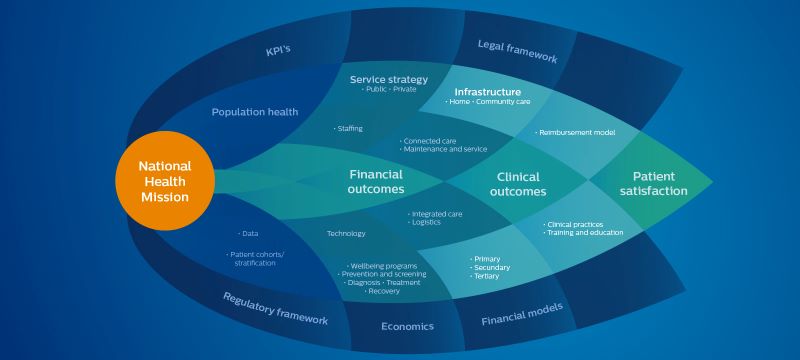
An empowered healthcare provider can transform itself from a complex quantity-based system into an outcome-based approach with a modern, digitally-fueled, user-centric network of connected experts, from hospitals and local health providers to insurance and technology companies. Still with the same passion, expertise and devotion – but with a shared sense of purpose, a reinvigorated idealism centered on what’s conceivable rather than merely achievable.
The bridge between these two convergent user and provider trends is mindset. Empowering patients to design a new way of extending life, while empowering governments and their stakeholders to redesign working practices.
The healthcare system revolution isn’t simply a technological one, it’s cultural too, in which consumers are no longer passive recipients of services. They are looking for ways to create new actions themselves.
In the past, patients were almost secondary figures, dwarfed by the mass-production ‘factories’ of care and treatment, where growing multimorbidity would mean being passed among different specialists. The system is buckling because it wasn’t designed for such care co-ordination.
Mass-customisation worked when numbers were manageable. But now, with rapidly-growing populations and ageing societies – combined with limited budgets – the system can’t cope.
Such a crisis means patients have to take ownership of their care. We see it most obviously with a new generation of elderly whose use of technology, coupled with their own active regimens, is enriching their lives. They have been liberated into taking control of their health in ways that were denied previous generations. They think across the entire healthcare continuum – from living with a condition to its diagnosis, treatment and recovery. And so it is beholden to us to collaborate on designing a future that reflects that – not just a system that deals with a part of your well-being and then passes you on.
Collaboration has usurped the patrician doctrine of ‘we know best’. Instead, we need to ask questions before even contemplating answers. That is where the paradigm of empowerment is critical – on connective partnerships that enable all parties to
co-create.
From those partnerships will emerge a new personalized, people-focused system of healthcare. At Philips we understand that to respond in a meaningful, holistic and agile way to people’s needs, we must analyze psychographic profiles not only of clinical conditions. That is why we fill our design teams with psychologists, sociologists, anthropologists – next to classic design capabilities – in order to construct customer-centric solutions that empower people to exert control over their lives.
We must accept that in the next few decades there won’t be enough healthcare services to support the population. That need not be a terrifying prospect – if we have the courage to ensure a new era of co-created strategic transformations that both user and provider desperately need.
There is no magic button. But a dramatic mindset change, influenced by design and innovation, can be effective. Delay is not an option. The challenges society faces are now not just in the future.